
Join 1,000s of women in our pause. community
Get valuable information and support from our community and team of menopause specialists. Subscribe for the latest evidence-based information, free events, helpful articles and inspiring women’s stories.
Downloaded from www.mymenopausecentre.com
Direct URL: https://www.mymenopausecentre.com/symptoms/muscle-aches-and-pain/
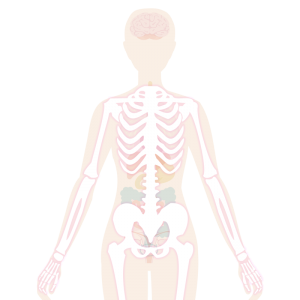
Loss of oestrogen can affect joints and the connective tissue that 'glues' your skeleton together. This can result in general muscle aches, pains and stiffness.
If you would like to learn more about the impact of your symptom(s) complete our free online menopause questionnaire here.
If you’re finding that your muscles often ache or feel sore, it could be another symptom of the menopause.
Telling the difference between muscle pain in the menopause and aches and pains from arthritis can be tricky. Of course, having aches and pains doesn’t mean you have arthritis, but it’s important to know when to ask for more help and advice.
During the menopause, women are more likely to get osteoarthritis (particularly in the hands) and rheumatoid arthritis. Osteoarthritis is a common condition causing joint pain and stiffness due to thinning or roughening of the cartilage covering the bone surface in the joint. Rheumatoid arthritis is an autoimmune disease. This means your immune system (which usually fights infection) mistakenly attacks the cells that line your joints, making the joints swollen, stiff and painful.
If you are experiencing joint pains, you may need to see a doctor, or other appropriate healthcare professional, and you may need to have some investigations done to get a diagnosis, depending on the symptoms you are experiencing.
Some conditions cause muscle aches specifically, such as:
This list is not exhaustive – please see a doctor if you have persistent muscle aches as your symptoms may need further investigation.

If you start to get aches and pains in the menopause, oestrogen is likely to play an important part. Oestrogen affects your cartilage (which is the connective tissue in joints) as well as the replacement of bone, and so plays a part in inflammation and pain. Replacing oestrogen with HRT has been shown to benefit all of these areas (see below for more on treatment)[1].
That said, the cause of your muscle aches may be unrelated to the menopause. Poor posture – particularly sitting in the same position looking at a screen, may be the culprit. Stress can also cause muscle tension and pain.
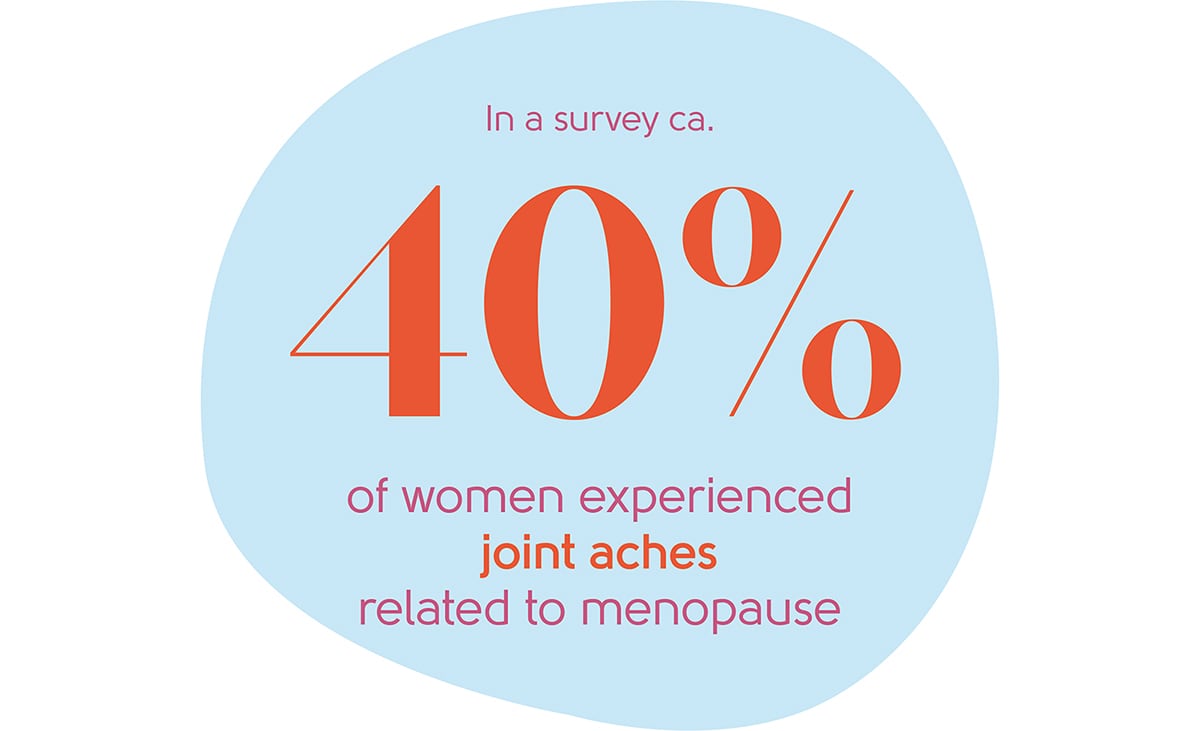
Musculoskeletal pain is common in the menopause – particularly joint aches. In one recent survey, joint aches were experienced by almost 40% of women aged between 45 and 65.
Muscle aches can occur at any stage of the menopause, including the perimenopause.
If you’re concerned about aches and pains or have swollen, stiff and painful joints, rashes, weight loss or if you feel unwell, we would advise you to see your GP to discuss your symptoms. They are likely to arrange further investigations and a referral to a specialist may be needed. If your joint is hot, red or swollen and you feel feverish and unwell, you should seek urgent medical attention by calling 999.
If your aches and pains are related to the menopause, there are several things that can help.
If you’re overweight or obese, weight control can help with musculoskeletal pain. Regular exercise, however gentle, can also help. It’s a good idea to start gently and gradually build up. Our friends at Her Spirit can help you find an activity and provide you with the motivation to do it.
Have a look at your working environment and try not to stay in the same position all day. Short breaks can help a lot.
Pain can feel worse if you are stressed, anxious or depressed. With that in mind, finding ways to improve your symptoms of stress, anxiety or depression could really help with aches and pains.
If sleep is an issue for you, working to improve this can help improve pain or help you to manage it. More information on sleep here.

Cognitive behavioural therapy can challenge negative thinking and help you break out of the vicious cycle of pain, low mood, stress and anxiety. Find out more about our CBT partners Sue Makin and Claire Lloyd.
Yoga helps you to relax your body physically, improving stretch and flexibility and could help muscle aches in this way. Pilates is another good way of improving strength and posture.
Seeing a physiotherapist could be a helpful option for you. A physiotherapist can advise on therapy through movement and exercise, targeting problem areas in your body to help restore movement and function if this is lacking.
There are over-the-counter medications that can help with your symptoms. These include:
Speak to your pharmacist or a doctor before trying painkillers, including anti-inflammatory medication. This is to make sure the medicine is safe for you and won’t interfere with other medicines you may be taking.
There’s evidence that HRT can help the musculoskeletal pains caused by the menopause. It can also be beneficial for arthritis[2]. We have treated women whose joint pains were their only symptom of the menopause, and they were helped by taking HRT.
HRT is the most effective way of managing menopause symptoms and improves the overall quality of life, energy levels and sleep.
You may feel anxious about taking HRT because of the well-publicised small risks, particularly of breast cancer. In reality, the risks are tiny for most. Lifestyle factors, like how much you weigh and how much alcohol you drink, can have a greater impact on your risk of breast cancer than HRT.
For most women, the benefits of menopause symptom control, reduction in risk of osteoporosis and heart disease far outweigh any small risks. You can find out more about HRT here.

If you’re concerned about muscle pain, talk to your GP. If you would like to discuss your symptoms in the context of the menopause, book an appointment with our menopause clinic but we would advise you to speak to your GP first to make sure that you do not need other investigations.
If you think you may be experiencing symptoms of the menopause transition, you can learn more with our symptom checker or by taking our Menopause Questionnaire.
You can also find more information about the menopause transition at the British Menopause Society and the National Institute for Health and Care Excellence. For more information on physiotherapy, have a look at the NHS.
Dr Clare Spencer
Registered menopause specialist, GP and co-founder; see Dr Clare in person at The Spire Hospital, Leeds or online
25/03/2025
We’ve created pause. as a space for women to come together and share stories about their menopause experience, ask questions, and to find support and inspiration. We'll also share the latest news and updates on the menopause from our experts.
Share your email to receive the latest news, updates and information on new products and treatments from My Menopause Centre and our pause. community. You can unsubscribe at any time.
We're committed to protecting and respecting your privacy - see our Privacy Policy and Terms and Conditions

Whether you want to discuss your symptoms, create a treatment plan that's right for you, understand some test results or have a check-up, the highly experienced doctors and nurses in our menopause clinic are here to help you.
Book nowSource: Roman-Blas JA, Castañeda S, Largo R, Herrero-Beaumont G. Osteoarthritis associated with estrogen deficiency. Arthritis Res Ther. 2009;11(5):241. doi:10.1186/ar2791.
Source: Magliano M. Menopausal arthralgia: Fact or fiction. Maturitas. 2010 Sep;67(1):29-33.