Downloaded from www.mymenopausecentre.com
Direct URL: https://www.mymenopausecentre.com/symptoms/hot-flushes-night-sweats/
Menopause, hot flushes and night sweats
Night sweats can happen without daytime flushes. Waking up drenched in sweat, with soaking sheets and night clothes can negatively affect sleep, adding to stress and anxiety.
Explore
Book an appointment
The highly experienced doctors and nurses in our menopause clinic are here to help you. Appointments from £190.
Book An AppointmentIf you would like to learn more about the impact of your symptom(s) complete our free online menopause questionnaire here.
What are hot flushes and night sweats?
Hot flushes and night sweats are two of the most well-known and experienced symptoms of the menopause. They are known as vasomotor symptoms. You may feel an intense heat spread over your body and become flushed and red. In addition, you may become sweaty or drenched in sweat.
They can vary in severity, frequency and duration, so for some women they happen regularly while others only experience the odd one here and there.
They generally last for a few minutes, sometimes shorter and sometimes longer. Some women experience them during the day, some just at night and some experience both. Night sweats can occur with or without daytime flushing.
During a hot flush or sweat, you may experience dizziness, heart palpitations or blushing. Flushes and sweats can occur spontaneously and may be triggered by various common situations, such as embarrassment, sudden room temperature change, stress, alcohol, caffeine or a hot drink.
Flushes and sweats can also dial up the severity of these menopause symptoms:
There’s evidence from around the world to suggest that the way society perceives the menopause and ageing can affect your experience of vasomotor symptoms[1]. In other words, if you live in a society that views the menopause and ageing in a positive light, how you experience your symptoms will be less severe than if you live in a society that views this negatively.
Hot flushes and work
Having hot flushes in the workplace brings its own set of worries. You may be dealing with work stress, which can make flushes worse, you may have to wear a uniform, and you may feel that you are unable to regulate the temperature of your working environment. It’s common to feel anxiety about being ridiculed by colleagues as well.
Studies have shown that women with problematic hot flushes and night sweats are more likely to consider giving up their jobs[2] – if you’re having these thoughts, you are not alone.
It’s really important that you’re able to find relief from your hot flushes. Try talking to your line manager or someone in your HR department – many companies now have policies in place for the menopause. The Faculty of Occupational Medicine has good guidance that you could share, as does the Chartered Institute for Personnel and Development.
What causes hot flushes and night sweats?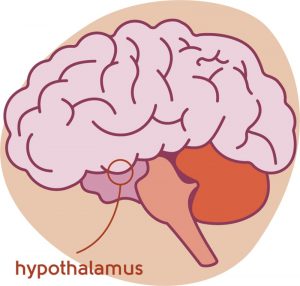
Vasomotor symptoms are widespread, but we still don’t fully understand them. It’s likely that oestrogen fluctuations trigger symptoms at the outset of the perimenopause or menopause. This results in a change to the temperature regulation in a part of the brain called the hypothalamus, so that small changes in the environment around you can trigger an extreme reaction. This is called a narrowing of the thermoneutral zone.
Oestrogen is not the only factor in the development of vasomotor symptoms. Other factors in the nervous system are likely to be involved, including serotonin and noradrenaline.
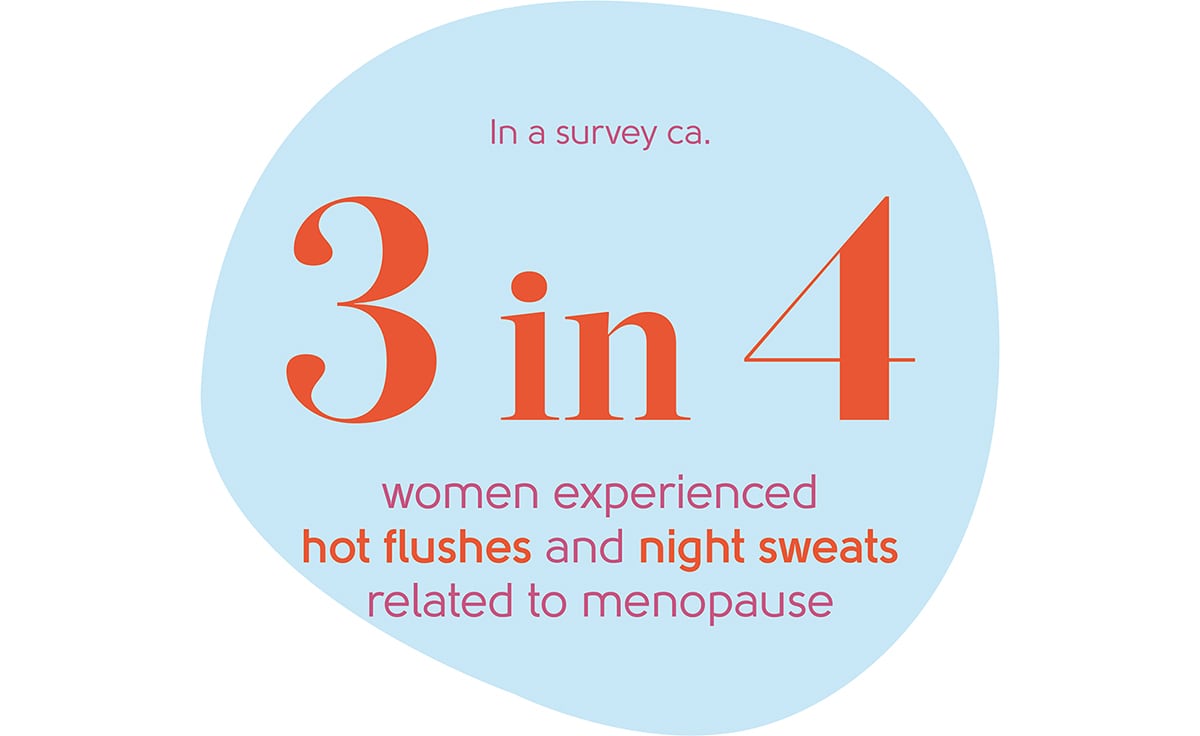
How many women typically experience hot flushes and night sweats?
Hot flushes and night sweats are experienced by approximately three quarters of women as they go through the perimenopause and menopause[12]. Around thirty per cent of women experience severe symptoms[3]. They usually last around eight years.
Around 40% of 60 to 65-year-olds still experience hot flushes and night sweats, and around twenty per cent of women experience symptoms for 15 years or more[13].
Are hot flushes and night sweats linked to any particular stage of the menopause?
Vasomotor symptoms start at any time in the perimenopause and can continue through the menopause and into postmenopausal life. They are most frequent in the first year after the last period.
How can hot flushes and night sweats be treated?
Management of these menopause vasomotor symptoms is not ‘one size fits all’. The good news is that there are many options to consider.
Practical top tips
- Loose clothes – they keep you cool and mean you don’t have to worry if you sweat
- Natural fibres – many clothes are made of natural fibres such as cotton, linen, bamboo and viscose, which are breathable
- Cotton in the bedroom – sleep in loose, light cotton nightwear and use cotton sheets instead of polycotton or man-made fibres
- Bedroom temperature – try to keep it cool. Maybe open a window
- Change of clothes – a spare set of nightclothes or a towel by the bed might be helpful
- Fans – they are a great help day and night
- Cooling sprays – you can buy cooling sprays specifically aimed at menopause flushes
- Work environment – speak to your employer – can you cool down the room temperature or open a window, or keep a fan at the ready?
You can read more about clothing tips for hot flushes and night sweats on our blog.
Lifestyle changes
Avoid triggers if you can – alcohol, caffeine, hot drinks and spicy food are the main culprits, but you may notice triggers specific to you.
 Stopping smoking can help too, as smoking can make hot flushes and night sweats worse[4]. The NHS is a great place to start if you need help quitting.
Stopping smoking can help too, as smoking can make hot flushes and night sweats worse[4]. The NHS is a great place to start if you need help quitting.
It’s easy to say exercise more and manage weight, and we know it can be a challenge – but there’s evidence that it can help with hot flushes[5].
Being overweight can make hot flushes and night sweats worse for some. The menopause transition can be a good time to look at your overall health and think about a plan to tackle your weight. It can be useful to focus on being healthy rather than simply losing weight (which we know is easier said than done). We offer support and advice through our friends at Her Spirit, who can help you find an activity you enjoy and provide the support to do it, and our nutritionist partner who can help with nutrition advice.
Hormone Replacement Therapy (HRT)
HRT is an oestrogen replacement therapy and it’s the most effective treatment for vasomotor symptoms for most women who take it[6]. The correct dose and how long you should take it for will depend on your symptoms.
You may feel anxious about taking HRT because of the well-publicised small risks, particularly of breast cancer. In reality, these risks are tiny for most. Lifestyle factors, such as how much you weigh and how much alcohol you drink, can have a greater impact on your risk of breast cancer than HRT.
For most women, the benefits of menopause symptom control, reduction in risk of osteoporosis and heart disease far outweigh any small risks.
You can find out everything you need to know about HRT here.

Alternative therapies
Herbal remedies can help some women. If you’re considering this route, we recommend looking for the THR mark, which stands for Traditional Herbal Registration. Registration to this scheme means that there is a guarantee that the goods bearing the mark meet certain defined standards or possess particular characteristics, as defined by the owner of the mark.
You can find more information about the THR mark here.
Black Cohosh – studies have shown that it can help with hot flushes. Although it may interact with blood pressure medicines and should not be taken by those women who are sensitive to aspirin or salicylates. It should never be taken by women taking Tamoxifen.
Sage – this can help relieve hot flushes. It shouldn’t be taken by those with high blood pressure.
Phytoestrogens – these are substances found in certain plants like soy, which can produce a weak, oestrogen-like effect on the body. There’s some evidence to suggest that women in countries where diets are traditionally rich in phytoestrogens experience fewer menopausal symptoms and have a lower rate of heart disease and osteoporosis[7].
Phytoestrogens can be taken as a supplement, such as red clover, or by increasing your intake of foods rich in them. Depending on your diet, you may need to radically change the way you eat to notice any effect. This is not recommended for women who have had breast cancer or other hormone-dependent tumours.
Soya, linseed oils and red clover are the richest food sources of phytoestrogen, others include:
- Cereals – oats, barley, rye, brown rice, couscous, bulgar wheat
- Seeds – sunflower, sesame, pumpkin, poppy, flax and linseed
- Pulses and beans – soya, chickpeas, kidney beans, haricot beans, broad beans and green split peas
- Vegetables – red onions, celery, sweet peppers, garlic, broccoli, tomatoes, bean sprouts
 Relaxation techniques
Relaxation techniques
Relax. It’s so easy to say, right? But it’s really important to remember to make time for what works for you. It might be yoga, relaxation breathing, meditation or anything else that helps you slow down. There are lots of great videos and apps out there that can help.
Talking therapies
There’s good evidence that cognitive behavioural therapy (CBT) can help decrease the severity and frequency of hot flushes. It can be a good alternative if you have been advised not to take HRT[8].
CBT is a therapy that helps you to challenge unhelpful and negative thoughts that get you in a vicious circle of thinking – and the outcome can improve your physical symptoms. For example, you may feel a hot flush starting and you may dread this happening because you’re at work and are embarrassed about what others will think.
As soon as the flush starts, you may start thinking negative thoughts, which may trigger a stress response that makes the physical hot flush worse.
CBT teaches you techniques to decrease stress, increase relaxation and challenge your thoughts. If you’re interested in learning more, you can find out about our CBT partners Sue Makin and Claire Lloyd.
Medication
If you don’t want to, or can’t take HRT, there are other medications that your doctor could prescribe.
Clonidine is a blood pressure tablet that is licensed for the treatment of hot flushes. It’s not a hormone and is not HRT.
Side effects of clonidine include dry mouth, drowsiness, dizziness, nausea and sleep interference. That said, it can help some women lead a normal life if they can’t or don’t want to take HRT. If you start clonidine and want to stop it, it’s important to stop it gradually over a week or so rather than immediately.
Antidepressants are not licenced for the treatment of vasomotor symptoms, but there’s evidence they may help[9]. Plus, they can also help with mood swings. Initial side effects include nausea, dizziness, short-term worsening of baseline anxiety and mood. It may help to start with a very low dose or even take it every other day.
See your doctor if your mood symptoms worsen significantly. Antidepressants can also affect your sex drive.
If you’re taking tamoxifen, there are certain antidepressants that you should not take, as they can make tamoxifen less effective. Venlafaxine (an SNRI) can be a good option if you’re taking tamoxifen. It can help hot flushes, improve mood and improve your quality of life, though initial side effects are common.
Gabapentin and pregabalin are also options. Side effects include dry mouth, drowsiness and dizziness, but they can improve sleep and help reduce hot flushes and sweats.
Veoza is a new medication licensed for the management of hot flushes and sweats. Veoza is the brand name for fezolinetant and works on the pathways in the brain responsible for the generation of hot flushes and sweats and studies have shown it’s around 60% effective at reducing the severity and frequency of vasomotor symptoms. Veoza is now available privately in the UK. Unfortunately, Veoza is not yet available on the NHS. To be available on the NHS, a further appraisal of the clinical and cost-effectiveness by the National Institute of Clinical and Healthcare Agency (NICE) is required. The publication date of this is yet to be confirmed. It is not recommended for women currently undergoing treatment for hormone dependent cancers and if you have a history of liver disease, you’ll need some tests beforehand. On the whole, it appears to be well tolerated. You can read more about Veoza here.
If you would like to discuss whether Veoza might be right for you, please book an appointment with one of the doctors in our clinic.
Hot flushes after cancer
Hot flushes can be a real issue for women who’ve been through breast cancer treatment. This is because treatments like chemotherapy, or removing the ovaries (oophorectomy), may force you into premature menopause if you weren’t already in the menopause transition.
Or you may have already been through the menopause when diagnosed with breast cancer. The hormone treatments can remove every last bit of oestrogen in your body so you may find hot flushes coming back or becoming more severe.
Hot flushes can be a side effect of many of the other treatments for breast cancer, such as tamoxifen, anastrozole, letrozole, exemestane and goserelin. Some women take hormone treatments to prevent breast cancer, including tamoxifen, anastrozole and raloxifene, or have their ovaries removed surgically.
Hot flushes can be more severe if you have experienced cancer treatments of oophorectomy than for women going through a natural menopause. They can result in more sleep issues and have a greater impact on your quality of life[10].
Treatment for other forms of cancer can also result in premature menopause, and again, hot flushes and night sweats can be more severe.
In terms of what to do, you may have been advised not to take HRT, depending on your type of cancer and circumstances. And some alternative medications may not be suitable for you, depending on which cancer treatments you’re taking. This is a discussion to have with your cancer specialist and menopause specialist because your individual circumstances are important.
There’s good evidence that cognitive behavioural therapy (CBT) can be effective in the treatment of hot flushes and night sweats, particularly when you have had breast cancer[11].
CBT therapy may be offered in cancer centres, through your GP, or through charities such as Maggie’s. There are good self-help resources out there as well, the Women’s Health Concern has good information.
What next?
As always, see your GP if you are concerned about hot flushes or night sweats. You can also book an appointment with our specialist menopause clinic.
If you think you may be experiencing symptoms of the menopause transition, you can learn more with our symptom checker or by taking our Menopause Questionnaire.
You can also find more information about the menopause transition at the British Menopause Society and the National Institute for Health and Care Excellence.
Authored by:
Dr Clare Spencer
Registered menopause specialist, GP and co-founder; see Dr Clare in person at The Spire Hospital, Leeds or online
Last updated:
07/11/2024
Book an appointment
The highly experienced doctors and nurses in our menopause clinic are here to help you. Appointments from £190.
Book An AppointmentLearn more
Join the pause. community
We’ve created pause. as a space for women to come together and share stories about their menopause experience, ask questions, and to find support and inspiration. We'll also share the latest news and updates on the menopause from our experts.
Want to be the first to hear our latest news? Join our pause. community today.
Share your email to receive the latest news, updates and information on new products and treatments from My Menopause Centre and our pause. community. You can unsubscribe at any time.
We're committed to protecting and respecting your privacy - see our Privacy Policy and Terms and Conditions

Book a consultation
Whether you want to discuss your symptoms, create a treatment plan that's right for you, understand some test results or have a check-up, the highly experienced doctors and nurses in our menopause clinic are here to help you.
Book nowReferences
-
Source: Longitudinal analysis of the association between vasomotor symptoms and race/ethnicity across the menopausal transition: study of women’s health across the nation. Gold EB, Colvin A, Avis N, Bromberger J, Greendale GA, Powell L, Sternfeld B, Matthews K Am J Public Health. 2006 Jul; 96(7):1226-35.
-
Source: Hardy C, Thorne E, Griffiths A, Hunter MS. Work outcomes in midlife women: the impact of menopause, work stress and working environment. Womens Midlife Health. 2018;4:3.
-
Source: Avis NE, Legault C, Coeytaux RR, Pian-Smith M, Shifren JL, Chen W, Valaskatgis P. A randomized, controlled pilot study of acupuncture treatment for menopausal hot flashes. Menopause. 2008 Nov-Dec;15(6):1070-8.
-
Source: Ziv-Gal A, Smith RL, Gallicchio L, Miller SR, Zacur HA, Flaws JA. The Midlife Women’s Health Study – a study protocol of a longitudinal prospective study on predictors of menopausal hot flashes. Womens Midlife Health. 2017;3:4. Published 2017 Aug 17. doi:10.1186/s40695-017-0024-8.
-
Source: Bailey TG, Cable NT, Aziz N, et al. Exercise training reduces the acute physiological severity of post-menopausal hot flushes. J Physiol. 2016;594(3):657-667. doi:10.1113/JP271456.
-
Source: National Institute for Health and Care Excellence. Menopause: diagnosis and management NICE guidelines [NG23] 2015https://www.nice.org.uk/Guidance/NG23 accessed Feb 2021.
-
Source: Prevalence of hot flushes and night sweats around the world: a systematic review. Freeman EW, Sherif K Climacteric. 2007 Jun; 10(3):197-214.
-
Source: Information for women Myra Hunter and Melanie Smith in collaboration with the British Menopause Society. Post Reprod Health. 2017 Jun;23(2):77-82.
-
Source: Review The role of serotonin in hot flushes. Berendsen HH Maturitas. 2000 Oct 31; 36(3):155-64.
-
Source: Hunter MS, Grunfeld EA, Mittal S, Sikka P, Ramirez AJ, Fentiman I, Hamed H. Menopausal symptoms in women with breast cancer: prevalence and treatment preferences. Psychooncology. 2004 Nov;13(11):769-78.
-
Source: Mann E, Smith MJ, Hellier J, Balabanovic JA, Hamed H, Grunfeld EA, Hunter MS. Cognitive behavioural treatment for women who have menopausal symptoms after breast cancer treatment (MENOS 1): a randomised controlled trial. Lancet Oncol. 2012 Mar;13(3):309-18.
-
Source: Bastian LA, Smith CM, Nanda K. Is this woman perimenopausal? JAMA. 2003 Feb 19;289(7):895-902.
-
Source: Gartoulla P, Worsley R, Bell RJ, Davis SR. Moderate to severe vasomotor and sexual symptoms remain problematic for women aged 60 to 65 years. Menopause. 2015 Jul;22(7):694-701.
Contact My Menopause Centre
- General enquiries: hello@mymenopausecentre.com
- Book appointments online: Log into your account and go to 'My appointments'
- Book appointments by phone: 0333 444 1067
- Website: https://www.mymenopausecentre.com