
Join 1,000s of women in our pause. community
Get valuable information and support from our community and team of menopause specialists. Subscribe for the latest evidence-based information, free events, helpful articles and inspiring women’s stories.
Downloaded from www.mymenopausecentre.com
Direct URL: https://www.mymenopausecentre.com/symptoms/anxiety/
A common symptom that leaves you feeling stressed, fearful or tense. It can cause physical symptoms, like palpitations, and can make symptoms like hot flushes worse.
The highly experienced doctors and nurses in our menopause clinic are here to help you. Appointments from £190.
Book An AppointmentIf you would like to learn more about the impact of your symptom(s) complete our free online menopause questionnaire here.
Experiencing anxiety is common during menopause. It’s an unpleasant symptom that can make you feel fearful or tense, and it can hit you suddenly or creep up slowly.
What’s important to remember is that anxiety is a normal human response to stressful situations. It starts to be an issue when it becomes hard to control your fear, making you feel stressed or overwhelmed, getting in the way of your ability to live life as you want to.
Anxiety might be the only symptom of the perimenopause and menopause that you experience. Many women don’t make the connection and just think that they aren’t coping like they used to.
If you are experiencing anxiety you certainly aren’t alone. Anxiety can happen to anyone – including those who’ve never experienced mental health difficulties before.
Anxiety can lead to physical symptoms such as:
During the perimenopause and menopause, a mixture of factors are happening at the same time, so it can be difficult to attribute the cause of your anxiety to one thing. Anxiety sometimes, but not always, goes hand in hand with low mood and symptoms of depression.
It’s important to understand that many mood changes can happen because of the hormone changes in your brain, and this is beyond your control – it’s not your fault or a sign that you are not coping. Just knowing this can, in itself, be helpful.
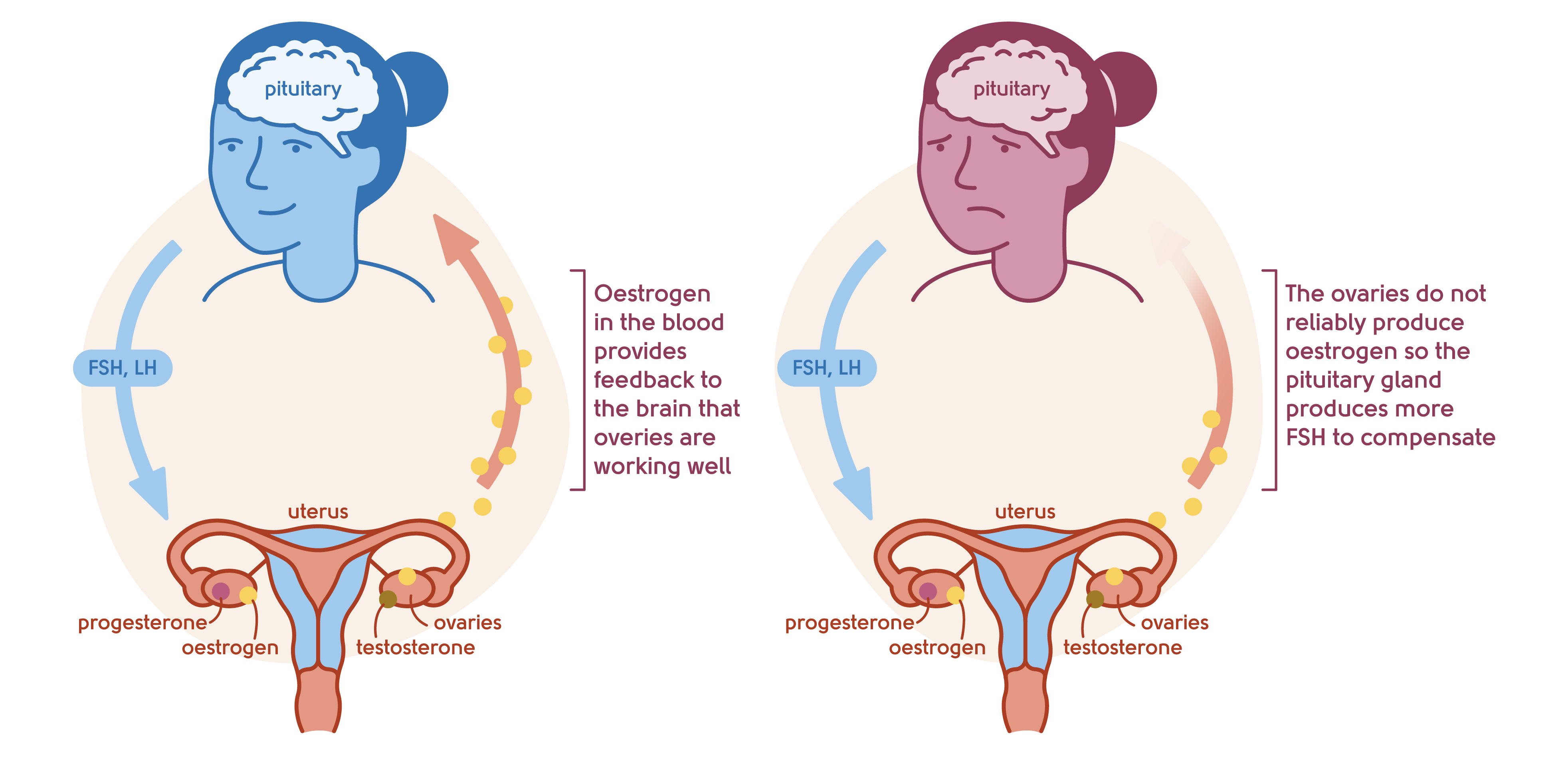
Illustration to show the feedback mechanism of the ovaries and the brain
Like depression, anxiety can occur because falling oestrogen levels change the way your brain functions. Studies[1] have shown that oestrogen is linked to levels of serotonin (the ‘happy hormone’) in the brain. There is evidence[2] that oestrogen levels are also linked to cortisol levels – the hormone of stress – so that when oestrogen levels drop, cortisol levels rise. It is likely that other hormones and chemical factors are also involved – the brain is complicated!
Some brains are more susceptible to the effects of changing hormone levels than others. You may be more likely to suffer from mood changes during the menopause if you’ve suffered from postnatal depression for example, and premenstrual syndrome can worsen in the perimenopause.
If you have already experienced a more severe form of anxiety disorder in the past, it’s important to be aware that this may get worse again as you go through the menopause transition.
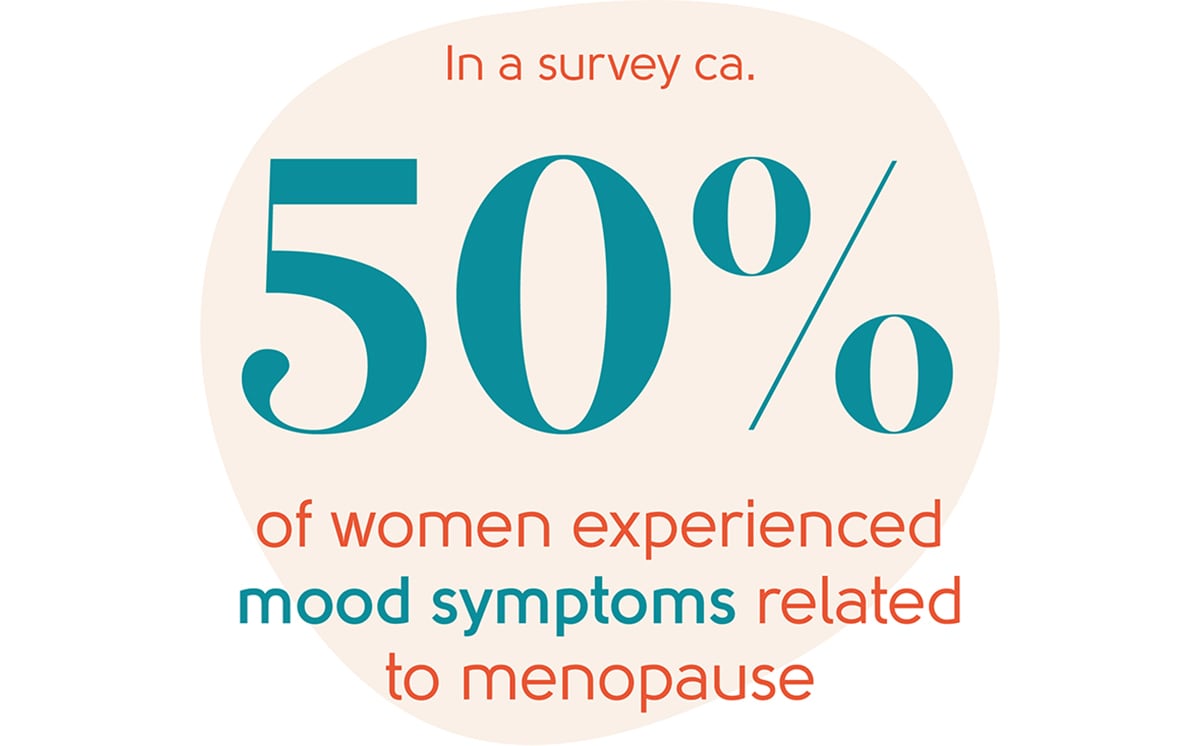
Anxiety is a common symptom of the menopause transition, with one survey showing that over half of the women interviewed (aged 45-65 and transitioning through the menopause) experienced mood changes[2].
Anxiety can occur at any stage of the menopause transition. It can creep in very early during the perimenopause before your periods have changed. It can start subtly and you may not realise that it’s related to the menopause – which is why it’s important to be aware of this symptom.
We know that anxiety can be worse during the perimenopause but we can’t say whether it will settle by itself. We urge you to seek help in managing your anxiety and, as you’ll see below, there are lots of different things you can do to manage this symptom.
The way forward to feeling better is different for everyone. Treatment and management options are similar to those that can help with the symptoms of depression.
When you go through the menopause, it’s so important to take very good care of yourself. Make sure you are allowing yourself to get enough sleep and exercise, and eat a healthy, balanced diet, limiting sugar and processed foods.
Give yourself the headspace to complete tasks and juggle what you need to juggle – we know that’s easier said than done at times!

Exercise can work wonders for anxiety in so many ways – it increases your sense of wellbeing, self-worth, body image and feelings of happiness, and it reduces your levels of stress and anxiety. If you are not exercising already, try looking at how you can add even the shortest amount to your day.
You may feel tired and low in energy and it may be the last thing you feel like doing. But just try putting on your trainers and walking outside even for five minutes – a short walk is better than not exercising at all and it can really help you to feel better.
The thought of relaxation can have the exact opposite effect on some women. It sounds easy but can sometimes be difficult and frustrating.
Our advice would be to try to find a practice that works for you. It might be yoga, breathing techniques, meditation or something else entirely. Here are our top apps for mindfulness and relaxation.

Counselling and cognitive behavioural therapy (CBT) help many women sort out how they are feeling. CBT can help break the vicious cycle of hot flushes and anxiety. Find out more about our CBT therapist partners Sue Makin and Claire Lloyd.
If your mood changes are related to the perimenopause and menopause, evidence indicates that HRT may improve your mood and anxiety[3]. It may be worth a try, even for a short period of time, to see if it helps. Many women find that they need to look at more than one approach to manage their symptoms – for example, HRT plus adding on yoga or exercise.
You may feel anxious about taking HRT because of the risks you’ve read about in the media, particularly of breast cancer. In reality, these risks are tiny for most women. Lifestyle factors, such as how much you weigh and how much alcohol you drink can have a greater impact on your risk of breast cancer than HRT. For most women, the benefits of menopause symptom control, reduction in risk of osteoporosis and heart disease far outweigh any small risks.
HRT does not press a pause button on the menopause. When you decide to stop HRT, you will feel how you would have felt at that age anyway. For example, if you were destined to experience hot flushes for eight years and you take HRT for three years, it’s likely you will continue to experience hot flushes when you stop it.
Most women can continue to take HRT for as long as they want. Knowledge is power. It’s important to understand the very small year-on-year risks (mainly breast cancer) and an annual discussion is important to review the benefits, any risks, or side effects and agree a plan for the year going forward.
Read about HRT here and see what you think.
Antidepressants also have a part to play in managing anxiety, particularly if you suffer from an anxiety disorder that’s unrelated to the menopause. Antidepressants can be taken as well as HRT if needed.
They can be helpful if you suffer from chronic anxiety disorder that worsens in the menopause transition. It’s important to speak to your doctor if this rings true for you.
Antidepressants can be helpful if your anxiety is getting in the way of your ability to live your life and if you don’t want to take HRT, or you have found HRT is not for you.
Antidepressants can take the edge off anxiety, help you sleep, and may also help with hot flushes. While very effective for many, antidepressants can have side effects – your doctor will discuss these with you. We recommend using antidepressants alongside lifestyle changes (such as exercise, reduction in alcohol intake) and therapy, as advised by your doctor.
You can find out more about antidepressants at Mind.
Wondering if HRT could help with your anxiety?
If you’re worried about anxiety, you should see your GP. To talk about anxiety in the context of the menopause, book an appointment with our menopause clinic.
If you think you may be experiencing symptoms of the menopause transition, you can learn more with our symptom checker or by taking our Menopause Questionnaire.
You can also find more information about the menopause transition at the British Menopause Society and the National Institute for Health and Care Excellence.
If you feel suicidal because of your anxiety please call your GP practice, the Samaritans, 111 or 999 straight away.
Dr Clare Spencer
Registered menopause specialist, GP and co-founder; see Dr Clare in person at The Spire Hospital, Leeds or online
06/11/2023
The highly experienced doctors and nurses in our menopause clinic are here to help you. Appointments from £190.
Book An AppointmentWe’ve created pause. as a space for women to come together and share stories about their menopause experience, ask questions, and to find support and inspiration. We'll also share the latest news and updates on the menopause from our experts.
Share your email to receive the latest news, updates and information on new products and treatments from My Menopause Centre and our pause. community. You can unsubscribe at any time.
We're committed to protecting and respecting your privacy - see our Privacy Policy and Terms and Conditions

Whether you want to discuss your symptoms, create a treatment plan that's right for you, understand some test results or have a check-up, the highly experienced doctors and nurses in our menopause clinic are here to help you.
Book nowSource: Rubinow, DR, et al. Naturally occurring changes in estradiol concentrations in the menopause transition predict morning cortisol and negative mood in perimenopausal depression. Clin Psychol Sci 2016; 4: 919–935.
Source: Menopause – Understanding the impact on women and their partners, Heather Currie, Sara J Moger (based on three online surveys with women 45+ with menopause symptoms (currently/in previous 10 years; 2015/n=1,000; 2016/ n=1,000; 2017/n=650 women and n=350 partners)
Source: NICE NG23 2015