Downloaded from www.mymenopausecentre.com
Direct URL: https://www.mymenopausecentre.com/gp-resources/what-is-the-right-balance-of-oestrogen-and-progestogen-when-taking-hormone-replacement-therapy-hrt/
What is the right balance of oestrogen and progestogen when taking Hormone Replacement Therapy (HRT)?
We are often asked 'What is the right balance of oestrogen and progestogen when taking Hormone Replacement Therapy (HRT)?' It is important to get the balance of oestrogen and progestogen right so that you only bleed once a month with sequential HRT, and so that you do not bleed at all with continuous combined HRT. In this article, Dr Clare Spencer, co-founder of My Menopause Centre, explains why and shares the latest guidelines from the British Menopause Society (BMS).
Explore

Combined HRT consists of two hormones, an oestrogen and a progestogen. Oestrogen is the hormone that helps manage symptoms. Oestrogen stimulates the lining of the womb (the endometrium) and can cause it to thicken. Some thickening of the womb lining is normal, but over-thickening increases the risk of cancer of the womb lining.
This is why, if you have not had a hysterectomy, you need to take a progestogen alongside the oestrogen. When taken appropriately, the progestogen helps prevent over-thickening and prevents cancer of the womb lining.
Sequential versus continuous combined HRT
With sequential combined HRT, you take oestrogen every day and the progestogen for half the month (usually a minimum of 12 days if taking micronised progesterone Utrogestan/Gepretix).
With continuous combined HRT both the oestrogen and the progestogen are taken every day. This is a no-bleed regime.
You start sequential HRT if it is within a year from your last period when you start HRT and you can take this for a maximum of 5 years. The maximum of 5 years is set as after this time there is an increased risk of cancer of the womb lining. When you reach the age of 55, the vast majority of women will have stopped bleeding so this is another time you would switch from sequential to continuous combined HRT. The exception to the rule is if you have a Mirena coil (or equivalent) fit. This gives a low constant dose of progestogen directly into the womb lining and is an effective way of stopping or significantly reducing bleeding even in the perimenopause.
You usually start continuous combined HRT if it has been around 1 year from your last bleed when you start HRT. Although you may have a little unscheduled bleeding when you start HRT – even a no-bleed HRT – this usually settles and so the aim with continuous combined HRT is not to have a bleed. (You can read more about postmenopausal bleeding here.)
What is the right balance of oestrogen and progestogen?
It is important to get the balance of oestrogen and progestogen right so that you only bleed once a month with sequential HRT, and so that you do not bleed at all with continuous combined HRT.
It is increasingly recognised, therefore, that as your dose of oestrogen increases you may need more progestogen to prevent unscheduled vaginal bleeding and potentially to prevent abnormal thickening of the womb lining.
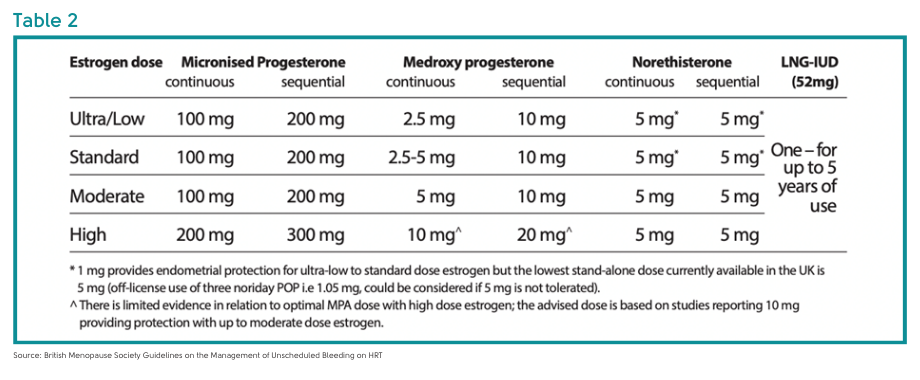
The next two tables are taken from the British Menopause Society Guidelines on the Management of Unscheduled Bleeding on HRT.
Table 1 shows how the doses of oestrogen are described as ultra-low, low, standard, moderate and high dose:
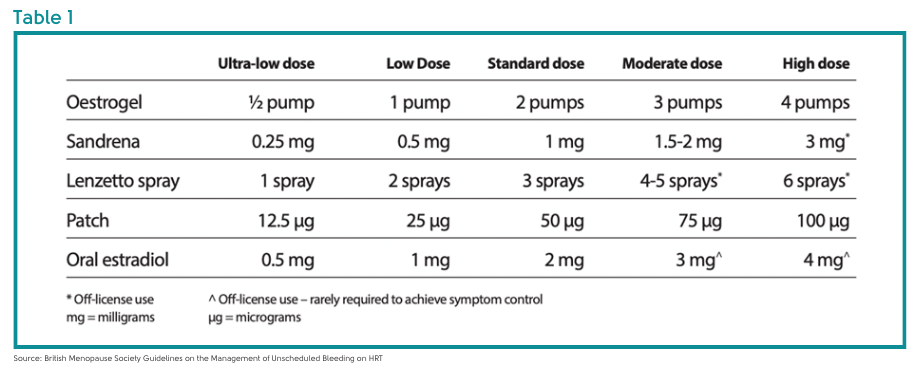 Table 2 shows the appropriate dose of progestogen according to whether you are taking ultra-low, low, standard, moderate and high dose oestrogen. You will see that you can use a Mirena coil up to and including a high dose of oestrogen, without the need for additional doses of progestogen:
Table 2 shows the appropriate dose of progestogen according to whether you are taking ultra-low, low, standard, moderate and high dose oestrogen. You will see that you can use a Mirena coil up to and including a high dose of oestrogen, without the need for additional doses of progestogen:
 We don’t have any data to tell us whether increasing the dose of progestogen has any impact on the risk of breast cancer.
We don’t have any data to tell us whether increasing the dose of progestogen has any impact on the risk of breast cancer.
These are not hard and fast rules. For example:
- If you have been taking Evorel 100 twice weekly with Utrogestan 100mg orally every night and if you have not had any bleeding, you may decide to stay on the Utrogestan 100mg rather than increase to 200mg with the advice of your doctor.
- If you have other risk factors for thickening of the womb lining or cancer of the womb lining you may be advised to increase the dose of progestogen.
Any prolonged or heavy bleeding or bleeding after sex should be reported to your doctor.
Risk factors for endometrial cancer with HRT
Major risk factors for endometrial cancer for women taking HRT are:
- Body mass index of 40 or more
- Genetic predisposition to endometrial cancer (e.g. Lynch or Cowden syndrome)
- Oestrogen only HRT for more than 6 months if you have a womb
- Only taking the progestogen part of your HRT every quarter for more than 12 months (tricycling)
- Sequential HRT for more than 5 years when started over the age of 45 yrs.
- 12 months or more of taking less than 12 days of micronsied progesterone every month, or less than 10 days of norethisterone every month as part of a sequential regime.
Minor risk factors for endometrial cancer for women taking HRT are:
- Body mass index 30-39
- Unopposed oestrogen (i.e. taking oestrogen without taking progestogen) for more than 3 months and less than 6 months if you have a womb
- Only taking the progestogen part of your HRT every quarter for less than 12 months (tricycling)
- Less than 12 months of taking less than 12 days of micronised progesterone every month, or less than 10 days of norethisterone every month as part of a sequential regime.
- When the progestogen dose is not in proportion to the oestrogen dose for more than 12 months
- Diabetes (you can read more about menopause and diabetes here).
- Having anovulatory cycles such as in polycystic ovarian syndrome
Unscheduled bleeding on HRT
It is common to bleed for the first 3 – 6 months on HRT as your body and womb lining settle. However, please speak to your doctor if you have any unscheduled bleeding so they can decide whether you need an examination and investigation. They may need to change the dose of progestogen, even if you are using a lower dose of oestrogen.
Unscheduled bleeding includes any bleeding on continuous combined ‘no-bleed’ HRT, or bleeding more than once a month, or having long or heavy withdrawal bleeds on sequential HRT.
Please speak to your doctor if you have any bleeding after sex, and always make sure that you go for your cervical smear when you are called.
If you’d like to learn more about HRT in general, check out this comprehensive article from Dr Clare Spencer here where she explains what it is, how to take it, the benefits, risks, and side effects; learn what is meant by bioidentical and body-identical hormones.
Authored by:
Dr Clare Spencer
Registered menopause specialist, GP and co-founder; see Dr Clare in person at The Spire Hospital, Leeds or online
Join the pause. community
We’ve created pause. as a space for women to come together and share stories about their menopause experience, ask questions, and to find support and inspiration. We'll also share the latest news and updates on the menopause from our experts.
Want to be the first to hear our latest news? Join our pause. community today.
Share your email to receive the latest news, updates and information on new products and treatments from My Menopause Centre and our pause. community. You can unsubscribe at any time.
We're committed to protecting and respecting your privacy - see our Privacy Policy and Terms and Conditions

Book a consultation
Whether you want to discuss your symptoms, create a treatment plan that's right for you, understand some test results or have a check-up, the highly experienced doctors and nurses in our menopause clinic are here to help you.
Book nowContact My Menopause Centre
- General enquiries: hello@mymenopausecentre.com
- Book appointments online: Log into your account and go to 'My appointments'
- Book appointments by phone: 0333 444 1067
- Website: https://www.mymenopausecentre.com