Downloaded from www.mymenopausecentre.com
Direct URL: https://www.mymenopausecentre.com/gp-resources/pelvic-organ-prolapse/
Pelvic Organ Prolapse
Are you experiencing pelvic organ prolapse and not sure where to turn for help? In this article Dr Surya Gupta-Wright, a menopause specialist and GP, provides valuable insight into what prolapse is and the different types, how it's diagnosed, common symptoms, and the various treatment options available.
Explore
Book an appointment
The highly experienced doctors and nurses in our menopause clinic are here to help you. Appointments from £190.
Book An AppointmentWhat is pelvic organ prolapse
The organs inside a woman’s pelvis include the womb (uterus), the bladder and the back passage (rectum). These are supported and held in position by the ligaments (fibrous tissues) and the muscles at the bottom of the pelvis which make up the pelvic floor.
Pelvic organ prolapse occurs when these normal support structures become weaker and consequently do not work properly. As a result of this one or more of the organs inside the pelvis can bulge into the vagina. This happens to different degrees, occasionally one of the pelvic organs can prolapse down so much that it protrudes beyond the opening to the vagina.
It is thought that over 40% of women are likely to suffer from some degree of pelvic organ prolapse in their lifetime.
Causes of pelvic floor prolapse
The main causes of pelvic floor prolapse are:
- Pregnancy and childbirth. It is more common in women who have had big babies, difficult and long labours or instrumental deliveries
- Increasing age due to the loss of some of the elasticity in the pelvic floor around the time of the menopause
- Being overweight
- Frequent straining due to long-term constipation, a long-term cough (smoking), or frequent heavy lifting
Symptoms of Pelvic Organ Prolapse
Some women may not have any prolapse symptoms, but a nurse or doctor may mention it when they are examined, e.g. for a smear test. Some women may experience no symptoms at all. Common symptoms include:
- Feeling a lump in your vagina, a dragging sensation, or ‘something coming down’. Some women might be able to feel or see a lump
- Some women may experience some discomfort in their vagina, lower back, or abdomen (tummy)
- Passing urine more frequently or leaking urine when coughing, laughing, and straining. Feelings that the bladder doesn’t empty properly or frequent urine infections
- Feeling that you cannot empty your bowels completely, needing to go to the toilet quickly, passing excessive wind, or leaking from the back passage. Some women need to push back on the back wall of the vagina to fully empty their bowels
Please let your doctor know if you are experiencing any change in your bowel or bladder habit.
- Sex may be uncomfortable or painful. A prolapse may affect arousal, and women may feel embarrassed and avoid having sex
Types of prolapse
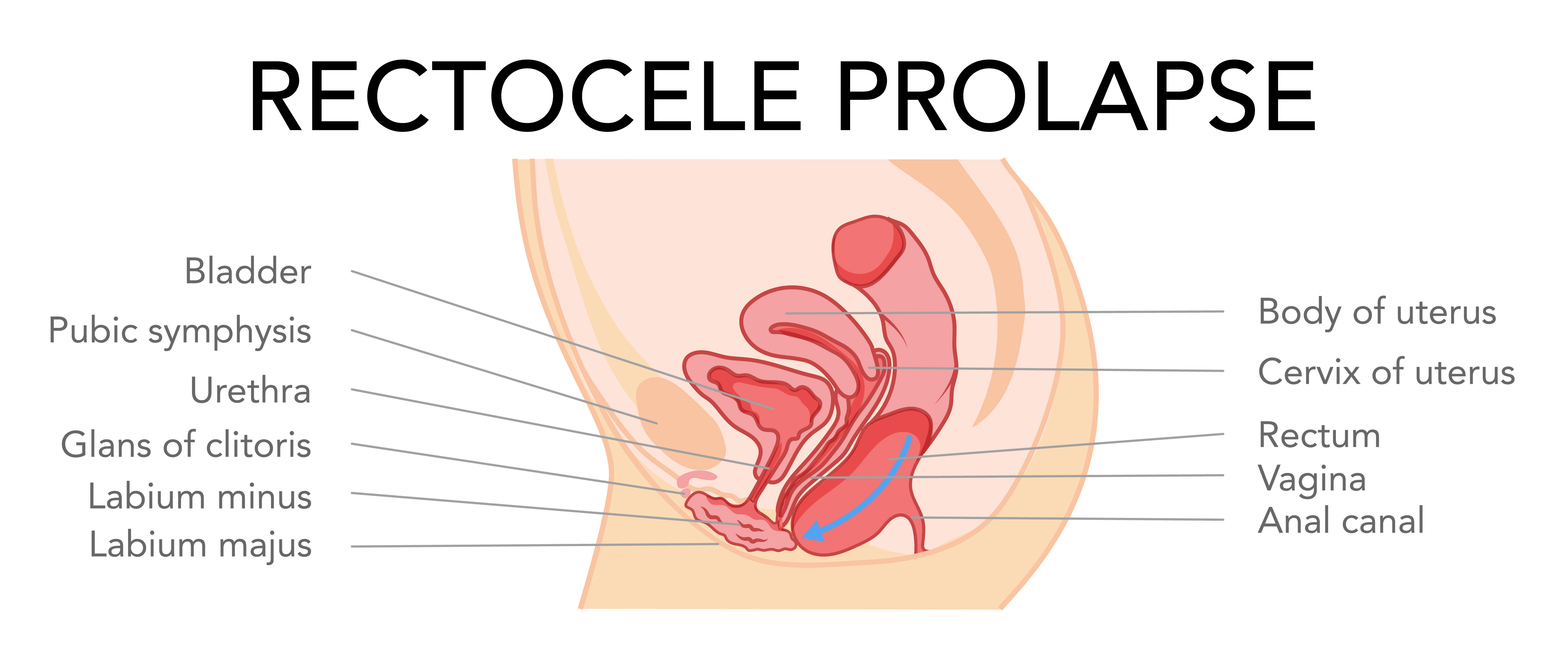
There are different types of prolapse depending on which pelvic organ or organs is prolapsing.
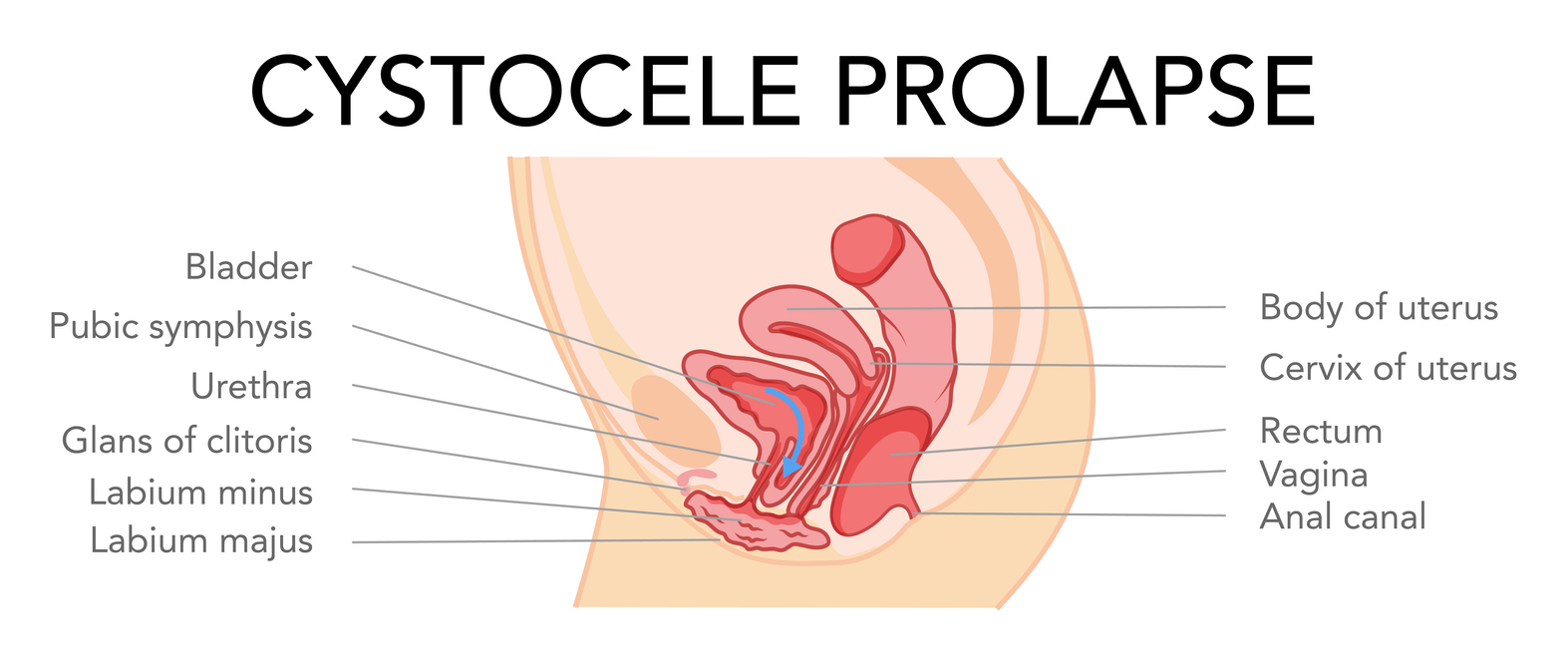
Anterior wall prolapse/Cystocele or cystourethrocele
This is when the bladder or urethra (the tube that you pee out of) bulges into the vagina. This is the most common type of prolapse.
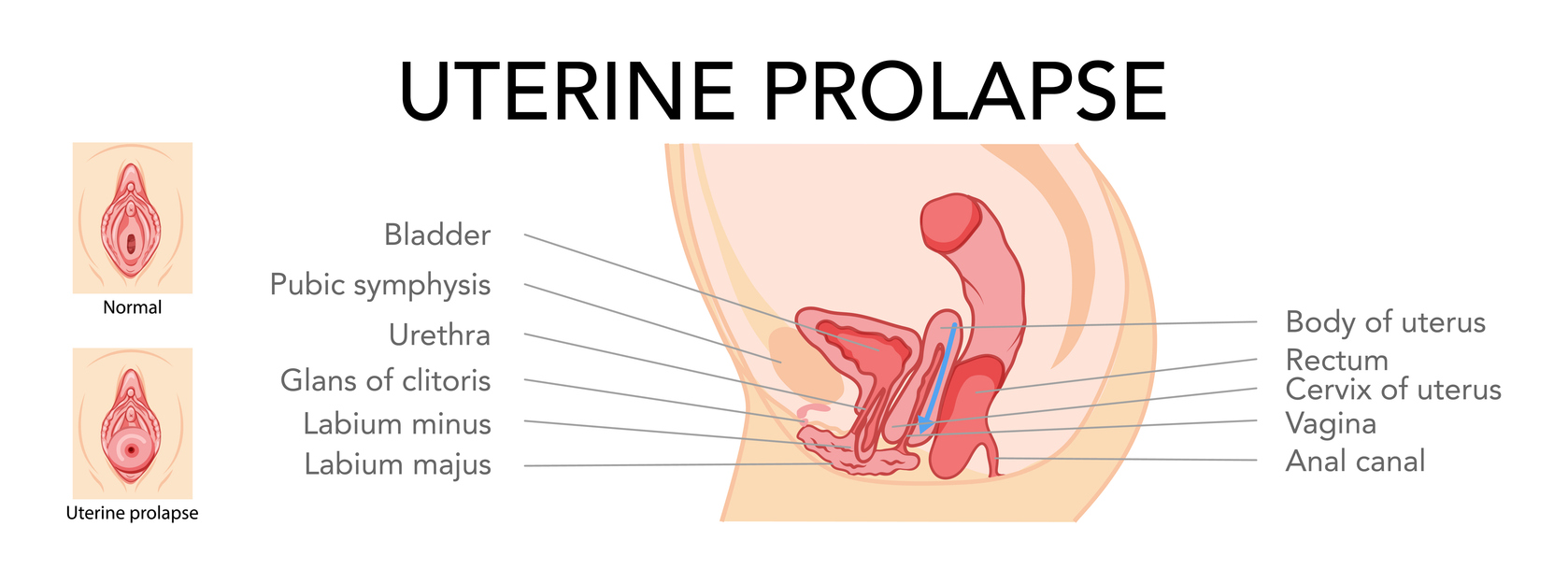
Uterine Prolapse or Vault prolapse
This is when the uterus sags down into the vagina and is the second most common type of prolapse. The uterus can sometimes protrude outside of the vagina and is called a procidentia.
Posterior wall prolapse/rectocele or enterocele
This is when the rectum or small bowel prolapse into the back wall of the vagina. This is the third most common type of prolapse.
After a hysterectomy (removal of the womb) the vault, or top of the vagina can prolapse down, this is called a vault prolapse.
How do you know if you have a prolapse?
Your doctor may need to examine you and, in doing so, may need to use a speculum (similar to the instrument used when you have a smear test). Your doctor may refer you for more tests on your bladder or bowel if they feel that it is necessary. These are often done in specialist clinics.
Treatment for a prolapse
You may choose not to have any treatment for your prolapse, particularly if it does not bother you. If you do want to manage your symptoms, there are a range of ways to do this:
Lifestyle changes
There may be some positive lifestyle changes that you can make:
- Losing weight, if you need to
- Stopping smoking
- Managing a chronic/long-term cough if you have one
- Avoiding becoming constipated, or treating your constipation
- Avoiding heavy lifting or particular types of exercise that might impact your pelvic floor
Pelvic floor exercises
Learning how to, and doing, regular pelvic floor exercises can be helpful. Seeing a specialist physiotherapist can be beneficial to make sure that you are doing the pelvic floor exercises properly. Regular pelvic floor exercises may help improve your symptoms or may prevent you from developing symptoms from your prolapse.
For more information on pelvic floor exercises, see this blog by physiotherapist and founder of Physiofastonline, Katie Knapton.
You may find this webinar, ‘Midlife Leaks and How to Manage Them’, also helpful.
Vaginal oestrogen treatment
Using vaginal oestrogen in the form of small pessaries, creams or a ring, can help the symptoms of a prolapse. The oestrogen helps to improve the elasticity of the pelvic tissues. Vaginal oestrogen is a form of HRT. Some women who cannot take HRT for medical reasons may still be able to use vaginal oestrogens, so talk to your doctor if you have any questions.
Vaginal support pessary
This is a plastic or silicone device (often ring-shaped) that fits into the top of the vagina. It can be fitted by a specialist doctor or nurse, and usually needs to be changed every 6 months. It can sometimes take a few tries to find the size and shape that is comfortable and works for you.
They usually do not cause any problems, but occasionally they can cause discharge, bleeding, or ulceration. This normally improves if the pessary is removed.
Some women who do not want surgery find these helpful. They can also be used if there is a long wait for an operation, or for women who have not yet completed their family.
Surgery
There are a number of different types of operations that can be done to improve a prolapse and reduce the symptoms that it causes. While most of the operations are done as vaginal surgery, there are a few procedures that may also involve abdominal surgery. You would need to be seen by a gynaecologist, or urogynaecologist. The specialist may ask you to make some of the lifestyle changes mentioned above before considering surgery. These will maximise your chances of successful surgery.
If you are worried about your pelvic floor or any of the symptoms mentioned in this article, speak to your GP or book an appointment to speak to Dr Surya or one of the other doctors or nurses in our clinic.
You can also find out more information about bladder symptoms and infections, and the pelvic floor, here:
Urinary incontinence and pelvic organ prolapse in women: management; NICE guideline (April 2019 – updated June 2019)
Pelvic floor dysfunction: prevention and non-surgical management; NICE guideline (December 2021)
Authored by:
Dr Surya Gupta-Wright
Registered Menopause Specialist and GP.
Last updated:
06/06/2024
Book an appointment
The highly experienced doctors and nurses in our menopause clinic are here to help you. Appointments from £190.
Book An AppointmentJoin the pause. community
We’ve created pause. as a space for women to come together and share stories about their menopause experience, ask questions, and to find support and inspiration. We'll also share the latest news and updates on the menopause from our experts.
Want to be the first to hear our latest news? Join our pause. community today.
Share your email to receive the latest news, updates and information on new products and treatments from My Menopause Centre and our pause. community. You can unsubscribe at any time.
We're committed to protecting and respecting your privacy - see our Privacy Policy and Terms and Conditions

Book a consultation
Whether you want to discuss your symptoms, create a treatment plan that's right for you, understand some test results or have a check-up, the highly experienced doctors and nurses in our menopause clinic are here to help you.
Book nowContact My Menopause Centre
- General enquiries: hello@mymenopausecentre.com
- Book appointments online: Log into your account and go to 'My appointments'
- Book appointments by phone: 0333 444 1067
- Website: https://www.mymenopausecentre.com